Monday, November 30, 2009
Bedside trick - Placing large bore IV in patients with suboptimal veins.
Firstly, a small-bore (20- to 24-gauge) hand or wrist IV started after applying a continuous-pressure tourniquet to the upper extremity. Without deflating the tourniquet, through the new IV, a crystalloid solution is given (50-60 mls), to distend all veins of the upper extremity. Now you can place a large bore catheter into the vein that wasn’t even there five minutes ago.
Friday, November 27, 2009
Thursday, November 26, 2009
Thursday November 26, 2009
Q: What is catamenial hemoptysis?
Answer: Hemoptysis that is recurrent and coincident with menses.
The cause is intrathoracic endometriosis, usually involving the pulmonary parenchyma but occasionally affecting the airways.
Previous Related Pearl: Catamenial pneumothorax
Wednesday, November 25, 2009
Initiation of Inappropriate Antibiotics - Fivefold Reduction of Survival in Septic Shock
Objective: Our goal was to determine the impact of the initiation of inappropriate antimicrobial therapy on survival to hospital discharge of patients with septic shock.
Methods: The appropriateness of initial antimicrobial therapy, the clinical infection site, and relevant pathogens were retrospectively determined for 5,715 patients with septic shock in three countries.
Results: Therapy with appropriate antimicrobial agents was initiated in 80.1% of cases. Overall, the survival rate was 43.7%.
- There were marked differences in the distribution of comorbidities, clinical infections, and pathogens in patients who received appropriate and inappropriate initial antimicrobial therapy.
- The survival rates after appropriate and inappropriate initial therapy were 52.0% and 10.3%, respectively.
- Similar differences in survival were seen in all major epidemiologic, clinical, and organism subgroups.
- The decrease in survival with inappropriate initial therapy ranged from 2.3-fold for pneumococcal infection to 17.6-fold with primary bacteremia.
- After adjustment for acute physiology and chronic health evaluation II score, comorbidities, hospital site, and other potential risk factors, the inappropriateness of initial antimicrobial therapy remained most highly associated with risk of death
Conclusions: Inappropriate initial antimicrobial therapy for septic shock occurs in about 20% of patients and is associated with a fivefold reduction in survival. Efforts to increase the frequency of the appropriateness of initial antimicrobial therapy must be central to efforts to reduce the mortality of patients with septic shock.
Reference: Click to get abstract
Initiation of Inappropriate Antimicrobial Therapy Results in a Fivefold Reduction of Survival in Human Septic Shock - CHEST November 2009 vol. 136 no. 5 1237-1248
Tuesday, November 24, 2009
Classic vs Delayed TRALI syndrome
Characteristics of the “classic TRALI syndrome” are:
- time of onset within 2 hours (usually up to 6 hours);
- rapid development;
- no other risk factors for ALI except transfusion;
- anti-neutrophil antibodies pathophysiology and
- onset after a single unit of blood product.
Characteristics of the “delayed TRALI syndrome” are:
- time of onset 6-72 hours after transfusion;
- slow development of clinical presentation;
- patients have other risk factors for ALI (i.e. sepsis, aspiration, near-drowning, disseminated intravascular coagulation, trauma, pneumonia, drug overdose, fracture, burns and cardiopulmonary bypass);
- two- step pathophysiology and
- common after massive transfusion (40-57%)
Monday, November 23, 2009
Bedside trick!
Scenario: You are inserting an emergent femoral central line in a severely vasculopath patient with exhausted upper vessels. Patient has previous history of IVC filter placement. What would be your worry?
Answer: Dislodgment of Inferior Vena Caval Filter.
Many cases have been reported in literature where IVC filters get dislodged by guidewires during the insertion of central venous catheters. 3 precautions/tricks can prevent this complication
- Limiting the distance that a guidewire is inserted into a vein during central line insertion.
- Inserting the straight end of the guidewire would also be effective.
- Inserting a smaller length central venous catheter (16 cm) instead of full 20 cm length central venous catheter.
Guidewire Dislodgment of Inferior Vena Cava Filters During Insertion of Central Venous Catheters - Vascular and Endovascular Surgery, Vol. 31, No. 5, 587-593 (1997)
Sunday, November 22, 2009
Acute organophosphate toxicity !
Normally, acetylcholinesterase catalyzes the degradation of the neurotransmitter acetylcholine in the synapse (yellow panel below). Organophosphate pesticides phosphorylate acetylcholine, thereby reducing the ability of the enzyme to break down the neurotransmitter (red panel below). This produces an accumulation of acetylcholine in the central and peripheral nervous systems, resulting in an acute cholinergic syndrome via continuous neurotransmission - called M-U-D-D-L-E-S:
- miosis,
- urination,
- diarrhea,
- diaphoresis,
- lacrimation,
- excitation of the central nervous system, and
- salivation

Saturday, November 21, 2009
Lets have some music in CCU !
Background: Most percutaneous coronary interventions are performed through the femoral artery. In order to stop bleeding and achieve homeostasis, a C-clamp is used after percutaneous coronary interventions. However, the experience is painful for patients and they inevitably suffer discomfort. Pain may lead to stress responses and may affect the physical and mental health of patients. One potential beneficial practice is having the patient listen to relaxing music, which might have the effect of reducing situational discomfort and pain.
Methods: A randomized controlled study was conducted during the period September 2004 to March 2005. Forty-three people (20 experimental and 23 control) were recruited from the intensive care units of two acute care hospitals in Hong Kong. Physiological and psychological variables were collected at baseline and at 15, 30 and 45 minutes.
Results:
- In the music group, there were statistically significant reductions (P = 0·001) in heart rate, respiratory rate, and oxygen saturation than the control participants at 45 minutes.
- In the music group, statistically significant reductions (P = 0·001) in systolic blood pressure, heart rate, respiratory rate and oxygen saturation were found at the four time points, but not in the control group.
- No statistically significant differences were found at baseline comparison of the two groups, but statistically significant differences in pain scores were found at 45 minutes for participants in the music group compared with the control group (P = 0·003).
- Participants in the control group showed statistically significant increases in pain at 45 minutes compared with baseline (P less than 0·001).
Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions: Journal of Advanced Nursing: Volume 53 Issue 6, Pages 669 - 679 - Published Online: 8 Mar 2006
Friday, November 20, 2009
CASCADE: Aspirin alone as effective as aspirin plus clopidogrel in preventing vein graft disease post-CABG
Aspirin alone is as effective as aspirin and clopidogrel in preventing vein graft disease after CABG, results of the CASCADE trial demonstrated, suggesting that the use of dual antiplatelet therapy is not supported in this population.
CASCADE researchers randomly assigned 113 patients undergoing primary multivessel CABG with at least two saphenous vein grafts to either 162 mg aspirin daily and 75 mg clopidogrel daily (n=56) or 162 mg aspirin daily and placebo (n=57). Primary outcome was vein graft intimal hyperplasia, with intimal area measured by IVUS. The study was powered for 20% clinically-relevant reduction with clopidogrel.
At one year, patency did not differ between the groups; overall patency was 95.2% in the treatment group and 95.5% in the placebo group (P=1.00).
Freedom from individual major adverse cardiac events – stroke, death and MI – and a composite of all three was similar in both groups (P=.76), as was major and minor bleeding (P=.02).
Source:
Kulik A. Presented at: American Heart Association Scientific Sessions 2009; Nov. 14-18, 2009; Orlando, Fla - http://www.theheart.org/article/1024575.do
Thursday, November 19, 2009
Q: Serum alkalinization with intravenous sodium bicarbonate has been the mainstay of therapy in (CA) cyclic antidepressants (amitriptyline, desipramine, imipramine, nortriptyline, doxepin, clomipramine, and protriptyline) overdose. What is the cutoff limit of QRS complex for use of intravenous sodium bicarbonate therapy?
Answer: A QRS of 100 milliseconds or greater is generally use as the cut off for intravenous sodium bicarbonate. Beside alkalinization, sodium loading may be the most important factor in the reversal of the symptoms of cyclic antidepressant toxicity. IV normal saline are indicated for CA-induced hypotension.
Wednesday, November 18, 2009
Q: Which patient is more hypoxemic?
Patient A: PaO2 85 mm Hg, SaO2 95%, Hb 7 gm%
Patient B: PaO2 55 mm Hg, SaO2 85%, Hb 15 gm%
Answer:
Calculate arterial oxygen content (CaO2) (SaO2 x Hb x 1.34) assuming PaO2 is constant
Patient A
CaO2 = .95 x 7 x 1.34 = 8.9 ml O2/dl
Patient B
CaO2 = .85 x 15 x 1.34 = 17.1 ml O2/dl
Patient A, with the higher PaO2, is more hypoxemic.
Full formula: Ca02 = (Hgb)(1.34)(Sa02) + (0.0031)(Pa02)
Tuesday, November 17, 2009
Q: What is the biggest danger while evaluating CXR with subcutaneous emphysema?
Answer: Missing underlying pneumothorax
The air may interdigitate with the muscle bundles to produce a characteristic linear streaky pattern, especially in the pectoralis muscles over the chest. When the streaky linear densities become widespread over the anterior and posterior chest walls, subcutaneous emphysema can obscure underlying pleural white line of a pneumothorax.

Monday, November 16, 2009
Q: What is the salvage treatment for severe pruritis in cirrhotic patient if all coventional and non-conventional treatment fails?
Answer: Plasmapheresis
References:
1. Plasmapheresis in the treatment of cholestasis-induced pruritus Ugeskr Laeger. 2006 Feb 20;168(8):779-81.
2. Role of plasmapheresis in the treatment of severe pruritus in pregnant patients with primary biliary cirrhosis: case reports - Can J Gastroenterol. 2008 May;22(5):505-7.
3. Plasmapheresis for the treatment of intrahepatic cholestasis of pregnancy refractory to medical treatment - American Journal of Obstetrics and Gynecology, Volume 192, Issue 6, Pages 2088-2089
Sunday, November 15, 2009
Saturday, November 14, 2009
How Wound V.A.C. Therapy System works
The V.A.C. Therapy System is comprised of three essential components that actively work together to help induce cellular wound healing through promotion of granulation tissue formation.
- V.A.C. Therapy Unit Provides intermittent and continuous therapy with integrated patient safety features
- SensaT.R.A.C.™ Technology Regulates pressure at the wound site to provide accurate delivery of prescribed therapy settings
- V.A.C. GranuFoam™ Dressings Help induce the necessary mechanisms to promote granulation tissue formation

How V.A.C. Therapy Works on the Cellular Level
Under negative pressure, V.A.C. Therapy with V.A.C. GranuFoam Dressings applies both mechanical and biological forces to the wound to create an environment that promotes wound healing. These forces are known as macrostrain and microstrain.
Macrostrain is the visible stretch that occurs when negative pressure contracts the foam. Macrostrain
- Draws wound edges together
- Provides direct and complete wound bed contact
- Evenly distributes negative pressure
- Removes exudate and infectious materials
Microstrain is the microdeformation at the cellular level, which leads to cell stretch. Microstrain:
- Reduces edema
- Promotes perfusion
- Increases cellular proliferation and migration
- Promotes granulation tissue formation
Friday, November 13, 2009
Central line complication

A 40-year-old man with Crohn's disease underwent an uncomplicated operation involving lysis of adhesions that were causing intestinal obstruction. After surgery, a cardiologist inserted a central venous catheter through the left subclavian vein. No problems with catheterization were noted. Three weeks later, after discharge, mild pain and edema developed in the patient's right lower leg. He was treated with antibiotics for 1 week, and his symptoms diminished. Six months after the operation, the patient presented with posterior cervical pain. A guide wire, presumably lost during the insertion of the central venous catheter, was protruding from the back of his neck (Panel A, arrow). A computed tomographic scan showed the fractured guide wire in the central venous system (Panel B, arrows). The wire protruding from the back of the neck was removed easily; however, it was difficult to remove the part of the wire involving the saphenous vein, and an open procedure with general anesthesia was required. The involved leg vein was thrombosed and occluded. At 1 year of follow-up, the patient was free of symptoms and signs.
Source:
Guo H, Lee JD, Guo M. Guidewire loss: mishap or blunder? Heart 2006;92:602-602
Thursday, November 12, 2009
Thursday November 12, 2009
Q: What percentage of patients may experience neurotoxicity from Amiodarone?
Answer: About 3%
Neurologic problems from Amiodarone use include tremor, gait ataxia, peripheral neuropathy, and cognitive impairment. The primary risk factor for amiodarone neurotoxic effects was duration of treatment, not age, drug dose, sex, or indication for therapy. Where this could be assessed, the adverse effects were usually but not always reversible.
Higher estimates of neurotoxic effects in the early amiodarone era may be related to a much higher daily dose.
Reference: click to get abstract
Frequency, Characteristics, and Risk Factors for Amiodarone Neurotoxicity - Arch Neurol. 2009;66(7):865-869
Wednesday, November 11, 2009
Sotalol and electrolytes
Calcium: Taking sotalol with a calcium dramatically reduces the absorption of the drug. Consequently, people who take a calcium supplement should take sotalol an hour before or two hours after the calcium.
Magnesium: Sotalol has a side effect of torsades de pointes. This side effect can be prevented by supplemental magnesium.
Potassium: Sotalol with hypokalemia have an increased risk of developing a serious heart arrhythmia. Therefore, special care should be taken when sotalol is prescribed with potassium-depleting diuretics.
Tuesday, November 10, 2009
Monday, November 9, 2009
Monday November 9, 2009
Q: What is the mechanism of action of B-blockers in reducing portal hypertension which ultimately help in reducing variceal bleeding?
Answer: Nonselective beta-blockers like propranolol and nadolol, reduce portal pressure through both local and systemic effects by 9% to 31%.
Local: In the splanchnic circulation, blockade of the vasodilating beta2 adrenoreceptors results in unrestricted alpha-adrenergic activity, splanchnic arteriolar vasoconstriction, and decreased portal inflow.
Systemic: Blockade of the cardiac beta1 receptors decreases the heart rate and cardiac output and secondarily decreases portal inflow.
Sunday, November 8, 2009
Sunday November 8, 2009
Q: Which medicine may transiently reverse hepatic encephelopathy?
Answer: flumazenil
GABA is a neuroinhibitory substance produced in the gastrointestinal tract. Of all brain nerve endings, 24-45% may be GABAergic. Increased GABAergic tone is observed in patients with cirrhosis, perhaps because of decreased hepatic metabolism of GABA.
When GABA crosses the extrapermeable blood-brain barrier of patients with cirrhosis, it interacts with supersensitive postsynaptic GABA receptors. The GABA receptor, in conjunction with receptors for benzodiazepines and barbiturates, regulates a chloride ionophore. Binding of GABA to its receptor permits an influx of chloride ions into the postsynaptic neuron, leading to the generation of an inhibitory postsynaptic potential. Administration of benzodiazepines and barbiturates to patients with cirrhosis increases GABAergic tone and predisposes to depressed consciousness.
The GABA hypothesis is supported by the clinical observation that flumazenil, a benzodiazepine antagonist, can transiently reverse hepatic encephalopathy in patients with cirrhosis.
Saturday, November 7, 2009
Naloxone for shock
Background: There is pre-clinical evidence, involving several animal species, suggesting that opioid peptides play a role in the physiopathology of shock (endotoxic, hypovolemic, cardiogenic, spinal, anaphylactic). Many case reports have suggested that naloxone (an opiate antagonist) might be an effective treatment for shock in humans, but others have not supported such a point of view. This controversy led us to undertake a meta-analysis of the available evidence on the efficacy of naloxone as a treatment measure for shock in humans.
Objectives: To evaluate the effectiveness and safety of naloxone in human shock and to estimate the methodological quality of the clinical trials.
Search strategy: We searched the Cochrane Injuries Group Specialised Register, CENTRAL (The Cochrane Library), MEDLINE (Ovid SP), PubMed, EMBASE (Ovid SP), ISI Web of Science: Science Citation Index Expanded (SCI-EXPANDED), and ISI Web of Science: Conference Proceedings Citation Index-Science (CPCI-S) (to December 2008). In order to identify further studies the reference lists of all included papers were examined and the primary investigators of eligible studies were contacted.
Selection criteria: Randomized controlled trials evaluating naloxone in human shock, regardless of the patient's age (adult, child, or neonate).
Data collection and analysis: Three independent review authors extracted data on study design, intervention, outcomes, and methodological quality.
Three independent readers reviewed 120 publications and selected six clinical trials. Overall agreement on study selection was perfect (concordance: 100%). The meta-analysis includes six studies involving 126 patients with septic, cardiogenic, hemorrhagic, or spinal shock.
Main results:
- Naloxone therapy was associated with statistically significant hemodynamic improvement (odds ratio 0.24; 95% confidence interval (CI) 0.09 to 0.68).
- The mean arterial pressure was significantly higher in the naloxone groups than in the placebo groups (weighted mean difference +9.33 mm Hg; 95% CI 7.07 to 11.59). No heterogeneity was found for this outcome.
- The death rate was lower in the naloxone group (odds ratio 0.59; 95% CI 0.21 was 1.67) but this was consistent with the play of chance. A significant heterogeneity was detected for the latter outcome (P less than 0.05).
Authors' conclusions: Naloxone improves blood pressure, especially mean arterial blood pressure. However, the clinical usefulness of naloxone to treat shock remains to be determined and additional randomized controlled trials are needed to assess its usefulness.
This is a Cochrane review abstract and plain language summary, prepared and maintained by The Cochrane Collaboration, currently published in The Cochrane Database of Systematic Reviews 2009 Issue 4, Copyright © 2009 The Cochrane Collaboration. Published by John Wiley and Sons, Ltd.. The full text of the review is available in The Cochrane Library.
This record should be cited as: Boeuf B, Poirier V, Gauvin F, Guerguerian AM, Roy C, Farrell C, Lacroix J. Naloxone for shock. Cochrane Database of Systematic Reviews 2003, Issue 3
http://www.cochrane.org/reviews/en/ab004443.html
Friday, November 6, 2009
On Use of NMB for the emergent tracheal intubation
Use of NMB is not routinely needed for the emergent tracheal intubation of inpatients who have received adjunct sedation. Emergent inpatient tracheal intubations, in which NMB had been utilized, were associated with a greater number of intubation attempts. The use of NMB, in only a subset of inpatients, may have been due to such issues as agitation, movement, or jaw clenching. These may have happened even with seemingly adequate levels of sedation. The observed association of NMB, with a greater number of tracheal intubation attempts, may actually have represented the failure to have successfully intubated with the use of sedation alone.
Clinicians need to be aware that the routine use of NMB may not be indicated for emergent tracheal intubations of inpatients who have received sedation. Although uncommon, the use of NMB may lead to catastrophic situations in which the patient can neither be intubated nor ventilated by mask. Additionally, breath sounds, transmitted via the tracheal tube during intubation, are lost with the use of NMB. Therefore, the advantages of intubating a spontaneously breathing patient are readily evident.
There is tremendous potential for hypoxia-related complications from the use of NMB. Consideration should be given to initially attempt those emergent inpatient tracheal intubations, which require sedation, without NMB. This is especially true in situations where additional trained personnel and airway management equipment are not readily available.
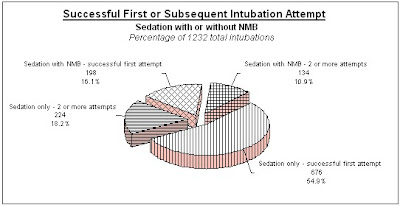
Intubation of Inpatients: A Retrospective Practice Analysis Comparing Adjunct Sedation With or Without Neuromuscular Blockade . The Internet Journal of Anesthesiology. 2003 Volume 7 Number 2
Thursday, November 5, 2009
Q: Define Massive Hemoptysis?
Answer: Traditionally 600 mL in 24 hours is a common definition of "massive hemoptysis" although a range of 200 to 1000 mL has been described. Since the actual volume is almost never measured, most physicians become concerned when an estimated 200 to 400 mL is expectorated and use this value as a definition of massive hemoptysis.
One reason to classify hemoptysis is to establish prognosis. Reported mortality in massive hemoptysis has ranged from less than 10% with intervention to 85% without intervention. Perhaps more important than expectorated volume is the rate of bleeding. Fortunately, massive hemoptysis is infrequent, with an incidence of less than 10%.
Wednesday, November 4, 2009
Low molecular weight protamine?
See following abstract
Heparin employed in cardiovascular surgeries often leads to a high incidence of bleeding complications. Protamine employed in heparin reversal, however, can cause severe adverse reactions. In an attempt to address this clinical problem, we developed low molecular weight protamine (LMWP) as a potentially effective and less toxic heparin antagonist.
A homogeneous 1880-d peptide fragment, termed LMWP-TDSP5 and containing the amino acid sequence of VSRRRRRRGGRRRR was derived directly from protamine by enzymatic digestion of protamine with thermolysin.
In vitro studies demonstrated that TDSP5 was capable of neutralizing various anticoagulant functions of both heparin and commercial low molecular weight heparin preparations. In addition, TDSP5 exhibited significantly reduced crossreactivity toward mouse sera containing antiprotamine antibodies. TDSP5 showed a decrease in its potential in activating the complement system. All of these findings suggested the possibility of markedly reduced protamine toxicity for TDSP5.
In this article, we conducted preliminary in vivo studies to further demonstrate the feasibility and utility of using LMWP as a nontoxic clinical protamine substitute. Dogs were chosen as test animals because they were known to magnify the typical human response to protamine. By using a full spectra of biological and clinical assays for heparin, including the anti-IIa and anti-Xa chromogenic assays and the activated partial, thromboplastin time and TCT clotting assays, TDSP5 showed that it could completely neutralize all these different anticoagulant functions of heparin in dogs. Although administration of protamine in dogs produced a significant reduction in mean arterial blood pressure (−14.9 mm Hg) and elevation in pulmonary artery systolic pressure (+5.0 mm Hg), the use of TDSP5 in dogs did not elicit any statistically significant change in any of the variables measured. Furthermore, the use of LMWP also significantly reduced the protamine-induced transient thrombocytopenic and granulocytopenic responses. The white blood cell counts and platelet counts decreased to 82.1% and 60.0% of baseline, respectively, in dogs given intravenous protamine compared to 97.8% and 88.6% of baseline in dogs receiving TDSP5. These preliminary findings indicated that LMWP could potentially provide an effective and safe means to control both heparin - and protamine-induced complications.
Reference: Click to get abstract
Low molecular weight protamine as nontoxic heparin/low molecular weight heparin antidote (III): Preliminary in vivo evaluation of efficacy and toxicity using a canine model - The AAPS Journal, Volume 3, Number 3 / September, 2001
Monday, November 2, 2009
Peramivir Fact Sheet for Health Care Providers
Source: http://www.cdc.gov/h1n1flu/eua/
As of October 23, 2009 as the request of the CDC the FDA authorized an Emergency Use of the investigational drug Peramivir, for the treatment of select adult and pediatric patients affected by the 2009 H1N1 influenza.
About Peramivir: It is an IV investigational neuraminidase inhibitor currently being evaluated in phase 3 clinical trials. Limited phase 2 and 3 safety and efficacy data are available, sufficient to allow emergency approval
Dosing: (adults) 600 mg IV once daily for 5-10 days
Renal adjustment needed: CrCl 50-60 ml/min 600mg IV daily; CrCl 31-49 ml/min 150mg IVdaily; CrCl 10-30 100mg IV daily; Hemodialysis or CrCl less than 10 ml/min 15 mg daily. Information is not available for those receiving peritoneal dialysis or CVVHD.
No hepatic dose adjustments needed.
Initial treatment course 5 or 10 days. Patients with critical illness may benefit from longer courses, no data available demonstrating increased efficacy
Administration: IV administration only. Infuse at a rate not to exceed 40mg/min. Dilute only in 0.9% sodium chloride. NOT compatible with dextrose solutions. Stable 24 hours refrigerated once constituted and diluted
Pharmacokinetics - T1/2: 7.7-20.8 hours
Warning/Precaution: not shown to reduce risk of transmission of influenza to others; should not be used in those with documented or highly suspected oseltamivir resistence; caution should be used in those with documented or highly suspected zanamivir resistence; In rare cases, peramivir may be associated with anaphylaxis an serious skin reactions, and a variety of neurologic and behavioral symptoms
Adverse events: diarrhea, nausea, vomiting, neutropenia are commonly reported in clinical trials. All medication errors and selected adverse events should be reported to the FDA Med Watch as this is still an investigational drug.
Sunday, November 1, 2009
Sunday November 1, 2009
Q: When the ascites is defined as Chylous?
Answer: True chylous ascites is defined as the presence of ascitic fluid with high fat (triglyceride) content, usually higher than 110 mg/dL.
In adults, chylous ascites is associated most frequently with malignant conditions like lymphomas and disseminated carcinomas from primaries in the pancreas, breast, colon, prostate, ovary, testes, and kidney. Tuberculosis, can infrequently be associated with chylous ascites.
Abdominal surgery is a common cause of chylous ascites. The surgical procedures most frequently associated with chylous ascites are resection of abdominal aortic aneurysm and retroperitoneal lymph node dissection.